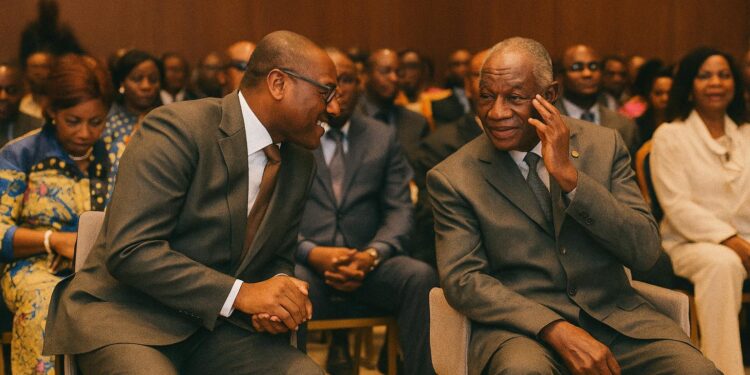
A strategic gathering in Brazzaville
The marble halls of the Ministry of Health in Brazzaville seldom feel as crowded as they did this week, when senior officials, academics and development partners opened the second ordinary session of the National Health Council. The three-day conclave comes at a pivotal moment: the Republic of Congo, like many emerging economies, is seeking to translate post-pandemic lessons into durable reforms while preserving macro-fiscal stability. By framing the debate around governance rather than isolated technical fixes, the organisers signalled an ambition to weave legal, managerial and financial threads into one coherent fabric.
Closing the gap to the Abuja target
Minister Jean Rosaire Ibara’s remarks were frank. At barely 4.2 percent of the national budget, public health expenditure stands far below the 15 percent threshold endorsed by African heads of state in Abuja in 2001. The consequence, he argued, is a system that cannot always anticipate epidemiological shocks or sustain quality improvements. International observers concur: the World Bank lists Congo’s current health spending per capita at just over 100 US dollars, less than half the lower-middle-income average (World Bank 2022). The minister nevertheless framed the situation as an opportunity, describing the council as a ‘laboratory for forward-looking solutions’ rather than a court of audit.
Innovative finance beyond the treasury
Delegates explored avenues that would diversify revenue without placing undue strain on the sovereign balance sheet. One proposal involves channelling corporate social responsibility funds from the oil and mining sectors into a dedicated health resilience facility. Another examines excise taxes on tobacco, alcohol and sugar-sweetened beverages—a measure that the WHO identifies as doubly beneficial because it raises resources while dissuading harmful consumption (WHO Fiscal Policies Report 2023). Public-private partnerships, particularly for hospital management and diagnostic services, were also dissected. The African Development Bank’s 2024 regional review notes that such arrangements in Côte d’Ivoire and Kenya have yielded efficiency gains of up to 20 percent, a precedent the Brazzaville meeting found compelling.
Human capital: the rural imperative
If financing is the bloodstream of a health system, personnel form its nervous system. Congo’s ratio of physicians, at 0.9 per 1,000 inhabitants, masks sharp geographic disparities (WHO Country Profile 2022). The council devoted considerable attention to incentives that could anchor clinicians in remote districts. Suggested levers include performance-based bonuses, subsidised housing and continuing-education fellowships. Participants drew inspiration from Rwanda’s ‘contractual approach’, where multiyear rural postings are tied to career advancement. The recent commissioning of two general hospitals—one in Brazzaville and a counterpart in Pointe-Noire—alongside 18 integrated health centres in rural areas provides the infrastructure backbone for such human-resource experiments.
Navigating a dual disease landscape
The epidemiological profile of Congo is bifurcated. Communicable diseases—malaria, tuberculosis and HIV/AIDS—remain endemic, yet noncommunicable ailments now account for nearly 45 percent of mortality. This transition, highlighted by the latest national health statistics and echoed in UNAIDS trend analyses (UNAIDS 2023), imposes a policy balancing act. On one side lie vertical programmes that rely on sustained donor funding; on the other, horizontal interventions such as hypertension screening and diabetes counselling that require strong primary care networks. Experts urged an integrated approach, in which community health workers perform simultaneous malaria tests and blood pressure checks, maximising each patient encounter.
Diplomacy, partnership and prudent optimism
The presence of Dr Vincent Dossou Sodjinou, WHO Resident Representative, underscored the multilateral stakes of the deliberations. He commended the government’s ‘pragmatic yet ambitious trajectory’, a formulation that resonated with diplomats in attendance. European Union envoys, for their part, expressed interest in aligning Global Gateway investments with Congo’s primary-care roadmap, while Chinese representatives noted that several provincial hospitals built through Sino-Congolese cooperation could host pilot telemedicine projects. By convening stakeholders under the statutory umbrella of the 1984 decree that created the National Health Council, Brazzaville delivered a message of institutional continuity even as it seeks renewal.
From resolutions to measurable impact
Veteran observers of African health summits know that eloquent communiqués do not automatically translate into altered patient outcomes. Yet there are reasons for guarded confidence. The Ministry of Finance has already scheduled a mid-term budget review that will apply the council’s recommendations to the 2025 appropriation bill. Meanwhile, the Chamber of Deputies is preparing amendments to the public-health code that would codify sin taxes and clarify the legal framework for public-private partnerships. Should these measures advance, Congo-Brazzaville might move closer to the Abuja benchmark while simultaneously strengthening rural service delivery. In the words of one senior official, quoted on background, ‘the test of our resolve will be written not in policy notes but in the life expectancy tables’. For now, the Brazzaville meetings have at least aligned the compass toward that distant but attainable horizon.